Glutathione Depletion and Diseases of the Eye: Cataract and Macular Degeneration
Author:- Ishika Jaitly
Cataract
A cataract [1-5] is an opacification of the lens and is the leading cause of blindness worldwide. The WHO estimates around 20 million people have bilateral blindness from cataracts. As longevity increases, the impact of cataracts on society is also expected to increase [6].
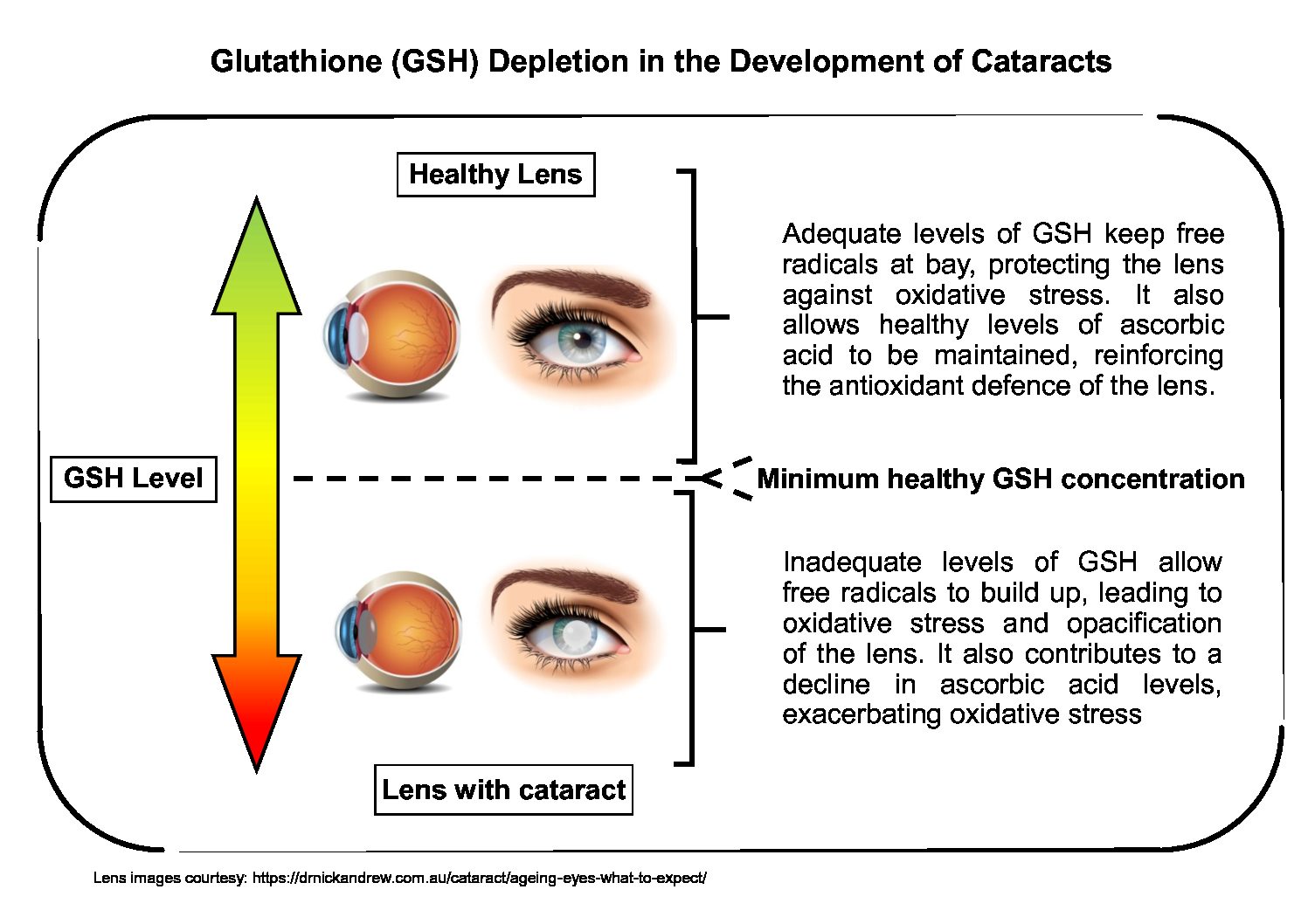
The three major risk factors in the development of cataracts are ageing, diabetes and exposure to sunlight [7,8], with ageing considered to be the most prominent [9]. While little can be done to modify the risk that advanced age poses, limiting exposure to sunlight is associated with a lower incidence of cataracts. Although not yet fully understood, the likely cause is the ionizing UV radiation spectrum of sunlight. This ionizing radiation promotes oxidative stress in the lens by producing damaging reactive oxygen species (ROS) [5]. Commonly known as free radicals, ROS are primarily quenched by the two principal components of the antioxidant defence system of the lens: Glutathione (GSH) and ascorbic acid [10]. Both are crucial in preventing the gradual loss of transparency of the lens [11], which is the classic symptom of cataracts.
During childhood, the lens possesses the highest levels of GSH of all tissues in the body [11]. However, with increasing age, GSH homeostasis becomes progressively dysfunctional in the centre of the lens [10]. Eventually, this results in chronically insufficient GSH levels to neutralize the ROS, leading to oxidative stress that damages lens proteins. The consequence is the formation of a cataract [10].
Another contributing factor to cataract formation is ascorbic acid, a powerful antioxidant that suffers from the same age-related decline as GSH [10]. Ascorbic acid serves to bolster the antioxidant defence and functional integrity of the lens [10,11]. Experimental evidence has demonstrated that a decrease in ascorbic acid levels is tied to GSH depletion [12]. Dehydroascorbate (DHA), an oxidant, is formed from ascorbic acid during the removal of ROS, yet the enzyme responsible for converting DHA back to ascorbic acid is dependent on GSH. Hence, a decline in GSH negatively affects this critical interconversion between ascorbic acid and DHA [8,10]. Diminishing ascorbic acid levels are inevitably accompanied by the toxic accumulation of DHA, leading to redox imbalance. The build-up of DHA favours the development of cataracts by exacerbating oxidative stress, eventually resulting in damaged lens proteins [8,9]. The fact that this redox imbalance occurs as a consequence of GSH depletion may explain why several clinical trials have provided no evidence of significant cataract prevention arising from the administration of high dosages of ascorbic acid [13]. Therefore, unless GSH levels in the lens are returned to optimal, supplementing with ascorbic acid is unlikely to offer any significant benefit.
Although cataract surgery is currently the primary treatment approach, it is very costly and often associated with complications. The reoccurrence of cataracts is, unfortunately, quite common. It can reasonably be predicted that cataract formation may be inhibited by maintaining an optimal concentration of GSH in the lens. Supplementation with gamma-glutamylcysteine (GGC) could provide the answer as it has been shown to increase cellular GSH above homeostasis effectively [14].
Macular degeneration
Macular degeneration is an eye disease that causes permanent vision loss. It is triggered by damage to the retinal pigment epithelium (RPE) of the eye resulting in overall blurred vision as well as loss of vision in the centre of the eye. It is a major concern in the elderly and is prevalent in most developed countries. Often, genetic factors predispose individuals to this disease, but unhealthy lifestyle choices such as poor diet or smoking, can also contribute to its development [15]. Since the exact risk factors may be hard to establish, treatment can be challenging [15].
Oxidative stress in the RPE, induced by ROS such as hydrogen peroxide, is hypothesized to be an important driving force in the progression of this disease [16]. This is unsurprising as the RPE has a high level of metabolic activity, and therefore oxygen demand, making it a significant source of ROS [17]. Mitochondria, which are structures within the cells of the RPE that act as energy powerhouses, are particularly susceptible to ROS-induced damage [17]. This further exacerbates ROS production and the ensuing oxidative stress [17], while also leaving the cells of the RPE with insufficient energy to divide and carry out their normal functions.
GSH is undoubtedly the most crucial component of the antioxidant defence of the eye. The chronic depletion of GSH, closely linked to ageing and diabetes, can precipitate cell death and impede cell division in the RPE via the mechanisms described above [18,19]. Increasing the pool of GSH in the RPE through supplementation with GGC [14], can potentially inhibit the progression of macular degeneration. Furthermore, GGC itself may be capable of directly acting as an antioxidant by supporting the activity of the enzyme GSH peroxidase [20], which is responsible for eliminating hydrogen peroxide in the RPE [21].
References
1. Giblin, F.J., Glutathione: a vital lens antioxidant. Journal of Ocular Pharmacology & Therapeutics, 2000. 16(2): p. 121-35.
2. Lou, M.F., Redox regulation in the lens. Progress in Retinal and Eye Research, 2003. 22(5): p. 657-682.
3. Beebe, D.C., and Y.-B. Shui, Progress in Preventing Age-Related Cataract, in Ocular Therapeutics, Y. Thomas, F.C. Abbot, and B.W. Martin, Editors. 2008, Academic Press: London. p. 143-165.
4. Shoham, A., M. Hadziahmetovic, J.L. Dunaief, M.B. Mydlarski, and H.M. Schipper, Oxidative stress in diseases of the human cornea. Free Radical Biology and Medicine, 2008. 45(8): p. 1047-1055.
5. Ho, M.-C., Y.-J. Peng, S.-J. Chen, and S.-H. Chiou, Senile cataracts and oxidative stress. Journal of Clinical Gerontology and Geriatrics, 2010. 1(1): p. 17-21.
6. Beebe, D.C., Y.-B. Shui, and N.M. Holekamp, Biochemical mechanisms of age-related cataract, in Ocular Disease, A.L. Leonard, et al., Editors. 2010, W.B. Saunders: Edinburgh. p. 231-237.
7. Lim, J.C., Arredondo, M.C., Braakhuis, A.J., and Donaldson, P.J., Vitamin C and the Lens: New Insights into Delaying the Onset of Cataract. Nutrients, 2020. 12(10): p. 3142.
8. Kisic, B., Miric, D., Zoric, L., Ilic, A., and Dragojevic, I., Antioxidant Capacity of Lenses with Age-Related Cataract. Oxidative Medicine and Cellular Longevity, 2012. 2012.
9. Truscott, R.J.W., Age-related nuclear cataract—oxidation is the key. Experimental Eye Research, 2005. 80(5): p. 709-725.
10. Lim, J.C., Grey, A.C., Zahraei, A., and Donaldson, P.J., Age‐dependent changes in glutathione metabolism pathways in the lens: New insights into therapeutic strategies to prevent cataract formation-A Review. Clinical and Experimental Ophthalmology, 2020. 48(8): p. 1031–1042.
11. Heruye, S.H., Nkenyi, L.N.M., Singh, N.U., Yalzadeh, D., Ngele, K.K., Njie-Mbye, Y., Ohia, S.E., and Opere, C.A., Current Trends in the Pharmacotherapy of Cataracts. Pharmaceuticals, 2020. 13(1): p. 15.
12. Meister, A., Glutathione-Ascorbic Acid Antioxidant System in Animals. Journal of Biological Chemistry, 1994. 269(13): p. 9397-9400.
13. Fernandez, M.M. and Afshari, N.A., Nutrition and the prevention of cataracts. Current Opinion in Ophthalmology, 2008. 19(1): p. 66-70.
14. Zarka, M.H. and Bridge, W.J., Oral administration of γ-glutamylcysteine increases intracellular glutathione levels above homeostasis in a randomised human trial pilot study. Redox Biology, 2017. 11: p. 631-636.
15. Lim, L.S., Mitchell, P., Seddon, J.M., Holz, F.G., Wong, T.Y., Age-related macular degeneration. The Lancet, 2012. 379(9827): p. 1728-1738.
16. Kularatne, R.N., C. Bulumulla, T. Catchpole, A. Takacs, A. Christie, M.C. Stefan, and K.G. Csaky, Protection of human retinal pigment epithelial cells from oxidative damage using cysteine prodrugs. Free Radical Biology and Medicine, 2020. 152: p. 386-394
17. Yang, M., So, K., Lam, W.C., and Lo, A.C.Y., Novel Programmed Cell Death as Therapeutic Targetsin Age-Related Macular Degeneration? International Journal of Molecular Sciences, 2020. 21(19): p. 7279.
18. Samiec, P.S., C. Drews-Botsch, E.W. Flagg, J.C. Kurtz, P. Sternberg, R.L. Reed, and D.P. Jones, Glutathione in Human Plasma: Decline in Association with Aging, Age-Related Macular Degeneration, and Diabetes. Free Radical Biology and Medicine, 1998. 24(5): p. 699-704.
19. Sun, Y., Zheng, Y., Wang, C., and Liu, Y., Glutathione depletion induces ferroptosis, autophagy, and premature cell senescence in retinal pigment epithelial cells. Cell Death & Disease, 2018. 9(7): p. 753.
20. Quintana-Cabrera, R., Fernandez-Fernandez, S., Bobo-Jimenez, V., Escobar, J., Sastre, J., Almeida, A., and Bolaños, J.P., γ-Glutamylcysteine detoxifies reactive oxygen species by acting as glutathione peroxidase-1 cofactor. Nature Communications, 2012. 3(718): p. 1-8.
21. Cohen, S.M., Olin, K.L., Feuer, W.J., Hjelmeland, L., Keen, C.L., and Morse, L.S., Low glutathione reductase and peroxidase activity in age-related macular degeneration. British Journal of Ophthalmology, 1994. 78(10): p. 791-794.

Another well explained & informative piece.. The diagram makes it even more easier to understand. Keep up the good work!!